At Melbourne ENT, located in St Kilda East, Victoria, we understand how persistent nasal symptoms such as rhinorrhea can significantly affect a person’s daily life, comfort, and wellbeing. Under the care of Dr Stephen Kleid and Dr Simon Braham, both expert ENT and head and neck surgeons, we provide advanced and compassionate care for patients experiencing chronic or unexplained nasal discharge.
Our clinic is equipped to handle a wide range of ENT concerns, and rhinorrhea is one of the more frequent reasons patients seek our specialised attention. Whether your runny nose is due to allergies, infection, or anatomical problems, we are here to offer clear answers and tailored treatment that works.
What is Rhinorrhea?

Rhinorrhea is the clinical term used to describe a runny nose, characterised by an excessive amount of fluid draining from the nasal passages. This fluid may vary in appearance – it might be thin and watery, thick and mucous-like, or occasionally discoloured depending on the underlying cause. While a runny nose is often considered a temporary nuisance associated with colds or allergies, chronic or unexplained rhinorrhea may signal a deeper issue that warrants thorough evaluation by an ENT specialist.
This condition can influence a wide array of related systems. Nasal discharge can block airflow, interfere with normal breathing, and impair your sense of smell. It can also lead to irritation in the throat due to post-nasal drip, and in some cases, contribute to ear symptoms through pressure or blockage of the Eustachian tubes.
When the source is structural, such as a deviated septum or enlarged nasal tissues, the symptoms may be long-standing and resistant to over-the-counter medications. Understanding and addressing the root cause is essential not only to symptom relief but also to preventing long-term complications.
DOWNLOAD GUIDE
Considering Rhinoplasty surgery? Information is just one click away.

Common Symptoms of Rhinorrhea
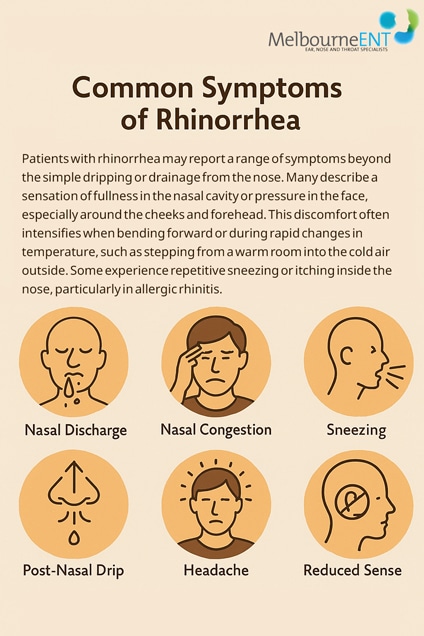
Patients with rhinorrhea may report a range of symptoms beyond the simple dripping or drainage from the nose. Many describe a sensation of fullness in the nasal cavity or pressure in the face, especially around the cheeks and forehead. This discomfort often intensifies when bending forward or during rapid changes in temperature, such as stepping from a warm room into the cold air outside. Some experience repetitive sneezing or itching inside the nose, particularly in allergic rhinitis.
The discharge may appear continuously or occur in episodes, and can alternate between nostrils. Others notice post-nasal drip, where mucus runs down the back of the throat, often leading to throat clearing, irritation, or a persistent dry cough.
In more advanced or long-standing cases, patients might suffer from headaches, facial tenderness, or even mild fevers – especially if the cause involves infection or sinus inflammation.
A diminished sense of smell or taste can also develop, impacting appetite and enjoyment of food. Sleep disturbances are not uncommon, particularly when nasal congestion or dripping intensifies at night. When rhinorrhea becomes a daily issue, it can be frustrating and socially disruptive, making prompt diagnosis essential.
Who is Affected by Rhinorrhea?
Rhinorrhea can affect individuals of any age, but certain groups are particularly vulnerable. In children, frequent viral infections, exposure to allergens in school or daycare settings, and enlarged adenoids can all contribute to chronic nasal symptoms. Children may also have difficulty articulating symptoms, which can delay treatment.
Adults often present with allergic rhinitis, structural nasal issues, or chronic exposure to environmental irritants such as pollution, cigarette smoke, or occupational chemicals. For some, non-allergic triggers such as perfume, changes in humidity, spicy food, or emotional stress can lead to reflex nasal discharge known as vasomotor rhinitis.
Older adults may experience age-related changes in the nasal mucosa that make the nose more sensitive to environmental changes. Additionally, medications for conditions such as high blood pressure or anxiety can lead to nasal dryness followed paradoxically by excessive mucus production.
Certain anatomical traits, such as a deviated septum or narrow nasal passages, can make people more prone to persistent symptoms. Likewise, patients with a history of sinus surgery or trauma to the nose may experience structural predispositions to chronic rhinorrhea.
Diagnosis and Evaluation at Melbourne ENT
At Melbourne ENT, every patient undergoes a comprehensive diagnostic process that begins with an in-depth clinical consultation. During this appointment, we take the time to understand the history of your symptoms, including how long you have experienced nasal discharge, what may trigger or worsen it, and what treatments you have already tried. We assess whether the condition is seasonal, persistent throughout the year, or varies with your environment or lifestyle.
A careful physical examination of the nose and surrounding structures helps us detect signs of inflammation, obstruction, or anatomical variations. We frequently perform a nasal endoscopy during the first visit.
This is a comfortable, in-office procedure using a slim camera to view the inside of the nasal passages and sinus openings. It allows us to identify issues such as polyps, enlarged turbinates, or unusual fluid flow patterns that might suggest a cerebrospinal fluid leak.
For patients with suspected allergies, we may recommend testing to identify specific allergens through skin or blood tests. In cases where sinus disease is suspected, especially if symptoms have persisted beyond ten days or recurred multiple times in the year, a CT scan may be requested to assess sinus anatomy and inflammation. If the nasal discharge appears to be one-sided and watery, and especially if it follows trauma or prior surgery, further tests may be needed to rule out a cerebrospinal fluid leak. Through this thorough process, we aim to pinpoint the cause of your rhinorrhea and create a plan that directly targets it.
Treatment Options for Rhinorrhea
Once we have identified the underlying cause, treatment is tailored specifically to your diagnosis and personal needs. For allergic rhinitis, we may recommend the use of modern intranasal corticosteroids, which are highly effective in reducing inflammation and controlling symptoms when used consistently. These are often complemented by oral antihistamines or newer nasal sprays that help reduce mucus production and prevent sneezing.
In cases of non-allergic rhinitis or vasomotor rhinitis, we may use targeted medications such as anticholinergic nasal sprays that specifically block the nerves responsible for overactive nasal discharge. For patients with recurring sinus infections, a course of antibiotics may be prescribed, sometimes alongside nasal rinses with saline to reduce congestion and flush out irritants.
Some individuals benefit from lifestyle adjustments such as using air purifiers, modifying their home environment to reduce allergens, or eliminating dietary triggers.
Patients who rely on over-the-counter decongestant sprays may need help weaning off these medications, as long-term use can worsen symptoms through a condition called rhinitis medicamentosa.
When medical treatment is ineffective or if there is a structural issue contributing to the problem, surgery may be recommended. This could include a septoplasty to straighten a deviated nasal septum, turbinoplasty to reduce the size of swollen nasal tissues, or endoscopic sinus surgery to improve drainage and airflow. All procedures are performed by our highly skilled surgeons with a focus on both functional improvement and patient comfort.
When is Surgery Recommended?
Surgical treatment is generally reserved for patients who have not responded to conservative therapies or who have anatomical causes that cannot be corrected with medication alone. If symptoms are severe, constant, or affecting your quality of life despite proper medical management, it may be time to consider a surgical solution.
In many cases, structural abnormalities such as a deviated septum or chronically enlarged turbinates restrict airflow and prevent proper drainage of mucus. Correcting these issues through procedures such as septoplasty or turbinoplasty can significantly reduce nasal discharge and improve breathing. If endoscopic examination or imaging reveals nasal polyps or chronic sinus inflammation, functional endoscopic sinus surgery (FESS) can be performed to clear these obstructions.
Recovery and Prognosis
Recovery varies depending on the treatment method, but the outlook for most patients with rhinorrhea is excellent. Those managed with medications often notice improvement within a week or two of beginning therapy. For allergy-related symptoms, long-term control may require seasonal adjustments or ongoing maintenance with nasal sprays and environmental strategies.
Surgical recovery is typically straightforward. Most nasal procedures are performed on a day-surgery basis with only mild discomfort and a short recovery period. You can expect some nasal congestion or minor bleeding for a few days post-operatively, but these symptoms resolve as healing progresses. Full recovery usually occurs within four to six weeks, with follow-up appointments to ensure proper healing and assess results.
Patients often experience a dramatic improvement in airflow, a reduction in discharge, and better sleep quality after successful surgical intervention. With appropriate follow-up and adherence to treatment plans, long-term control of rhinorrhea is highly achievable.
Risks or Complications if Left Untreated
Although often dismissed as a minor annoyance, chronic or unexplained rhinorrhea should not be ignored. Left untreated, persistent nasal discharge can lead to complications such as repeated sinus infections, worsening allergic inflammation, or the development of chronic cough due to post-nasal drip. It may also contribute to poor sleep, fatigue, and reduced productivity.
In some rare but serious cases, rhinorrhea could be the sign of a cerebrospinal fluid leak or a hidden nasal mass. These conditions require urgent medical attention, and early diagnosis can significantly impact the outcome. Addressing rhinorrhea promptly ensures not only symptom relief but also protects against long-term health consequences.
FAQs About Rhinorrhea
Can a runny nose be caused by something other than allergies or a cold?
Yes. While allergies and viral infections are common causes, rhinorrhea can also result from structural nasal issues, non-allergic rhinitis, environmental irritants, hormonal changes, and even neurological reflexes triggered by things like bright lights or strong emotions.
Why does my nose run more when I eat, exercise, or step outside?
This type of rhinorrhea is often related to non-allergic or gustatory rhinitis. It’s a reflex reaction triggered by temperature changes, certain foods (especially spicy or hot ones), or physical activity. It’s not related to infection or allergy and may require different treatments.
Is it normal for only one side of my nose to run?
A runny nose that is consistently one-sided may suggest a structural issue, nasal polyp, or in rare cases, a cerebrospinal fluid (CSF) leak. It’s important to have this properly assessed, especially if the discharge is clear, watery, and persistent.
Can a deviated septum cause a runny nose even if I don’t feel blocked?
Yes. A deviated septum can disrupt normal nasal airflow and mucus drainage, leading to irritation or compensatory overproduction of mucus. Even in the absence of noticeable blockage, this can contribute to chronic rhinorrhea.
Why do over-the-counter decongestants make my nose worse over time?
Prolonged use of topical decongestant sprays (like oxymetazoline) can cause a rebound effect called rhinitis medicamentosa. This condition leads to worsening congestion and increased nasal discharge once the medication wears off, creating a dependency cycle.
I’ve had a runny nose for months but no other symptoms – should I still see an ENT specialist?
Absolutely. Chronic rhinorrhea without obvious triggers may be due to anatomical changes, non-allergic rhinitis, medication effects, or less common underlying causes. An ENT evaluation can help uncover the source and offer targeted treatment options.
How does Melbourne ENT diagnose rhinorrhea if it seems like such a vague symptom?
We take a structured and evidence-based approach that includes history-taking, nasal endoscopy, allergy testing, and imaging when needed. We assess structural, inflammatory, and neurological contributors to ensure no aspect of the symptom is overlooked.
Sources:
- Allergic Rhinorrhea: Prevalence, Severity, and Risk Factors among Students at University of Nigeria, Enugu Campus
https://www.saspublishers.com/media/articles/SJMCR_136_1402-1407c.pdf - Contemporary Management of Cerebrospinal Fluid Rhinorrhoea: A Review of the Literature
https://www.mdpi.com/2077-0383/14/3/995 - Recurrent Cerebrospinal Fluid Rhinorrhea Secondary to a Seizure-Induced Skull-Base Defect: An Unusual Complication of Epilepsy
https://pmc.ncbi.nlm.nih.gov/articles/PMC12178260/ - Allergic Rhinitis – StatPearls – NCBI Bookshelf
https://www.ncbi.nlm.nih.gov/books/NBK538186/ - Unilateral Clear Thin Rhinorrhea: How Often Is It a Cerebrospinal Fluid Leak?
https://journals.sagepub.com/doi/10.1177/00034894251338895 - Expert Consensus on Nasal Anticholinergics in the Treatment of Rhinorrhea
https://journals.lww.com/ijsgh/fulltext/2025/01000/expert_consensus_on_nasal_anticholinergics_in_the.1.aspx - Effectiveness of Endoscopic Surgery for Treating Spontaneous Cerebrospinal Fluid Rhinorrhea
https://www.sciencedirect.com/science/article/pii/S2214751925000453
Concerned About Rhinorrhea?
If you are tired of living with a constant runny nose or feel your symptoms are getting worse, the team at Melbourne ENT is here to help. With decades of combined experience, Dr Stephen Kleid and Dr Simon Braham provide expert care grounded in thorough diagnosis, tailored treatment, and compassionate follow-up.
To schedule your consultation, contact our clinic at (03) 9038 1630 / (03) 9038 1311.
Experience relief from your symptoms and regain control of your health – starting with a single consultation.
Further Reading
- Read about Melbourne ENT’s Nose Concerns and Conditions
- Read about Melbourne ENT’s Surgery For Nasal Obstruction Melbourne
- Read about Melbourne ENT’s Allergic Rhinitis Melbourne
- Read about Melbourne ENT’s Nasal Congestion Melbourne


