
At Melbourne ENT, based in St Kilda East, Victoria, we are committed to providing comprehensive, specialist care for a wide range of ear, nose, throat, and head and neck conditions. Our clinic is led by two of Victoria’s most experienced ENT surgeons, Dr Stephen Kleid and Dr Simon Braham. Both are Fellows of the Royal Australasian College of Surgeons (FRACS) and renowned for their expertise, precision, and patient-centred approach. One of the most common conditions we treat, especially in children, is Middle Ear Infection, medically known as Acute Otitis Media (AOM). This condition can cause discomfort, affect hearing, and even impair speech and learning if left untreated. At Melbourne ENT, we diagnose and manage middle ear infections using the latest techniques and evidence-based care.
What Is A Middle Ear Infection?
A middle ear infection, or Acute Otitis Media, is an inflammation and infection of the space located behind the eardrum known as the middle ear. This space is typically filled with air and plays a critical role in sound transmission. When the Eustachian tube – a narrow passage connecting the middle ear to the back of the throat – becomes blocked due to a cold, allergy, or sinus infection, fluid can accumulate. This fluid creates an ideal environment for bacteria or viruses to grow, leading to an infection.
Middle ear infections can cause sudden and intense symptoms, particularly in infants and young children whose Eustachian tubes are shorter and more horizontal, making them more prone to blockage. While the majority of cases are acute and resolve with appropriate treatment, recurrent or chronic infections can result in hearing loss and other complications.
Common Symptoms Of Middle Ear Infection
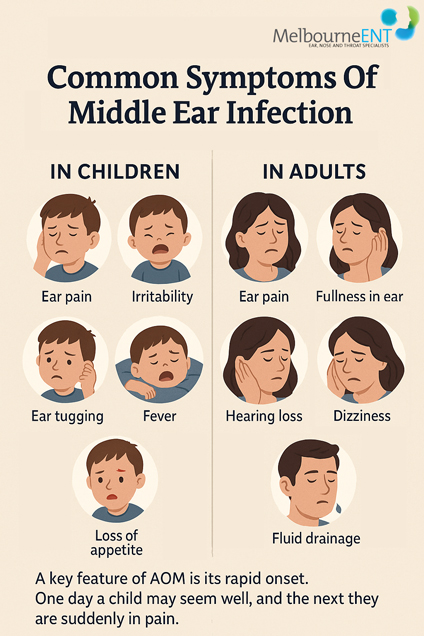
Middle ear infections present with a variety of symptoms, depending on age and severity. In children, symptoms often include unexplained irritability, frequent crying, difficulty sleeping, and ear tugging. These behavioural cues are frequently accompanied by more noticeable signs such as ear pain, fever, and a loss of appetite. Parents may observe that their child is less responsive to sound or struggling with balance.
In older children and adults, the symptoms tend to be more straightforward. Patients typically experience sharp or throbbing pain in the affected ear, a sense of fullness or pressure, temporary hearing loss, and occasionally fluid drainage from the ear if the eardrum has ruptured. Some may also experience mild dizziness or vertigo, especially if the inner ear is affected.
A key feature of AOM is its rapid onset. One day a child may seem well, and the next they are suddenly in pain. This sudden change can be distressing for families, but timely medical evaluation can lead to fast and effective relief.
Who Is Affected By Middle Ear Infections?
Acute Otitis Media can affect anyone, but certain groups are far more susceptible. Children between the ages of six months and three years are at the highest risk. Their developing immune systems and smaller, more horizontal Eustachian tubes make them more vulnerable to middle ear infections. The risk is further increased in children who attend daycare, use pacifiers, or are bottle-fed while lying down.
Environmental and anatomical factors also play a role. Exposure to tobacco smoke, whether direct or secondhand, significantly increases the risk. Children with allergies, sinusitis, or enlarged adenoids are also more likely to suffer from repeated infections. A family history of ear infections can further heighten susceptibility.
In adults, recurrent or chronic AOM can occur due to underlying sinus conditions, allergic rhinitis, or anatomical abnormalities. Smokers and those with compromised immune systems may also be at higher risk. Although less common in adults, when AOM occurs it can be quite painful and disruptive, particularly if associated with upper respiratory tract infections or changes in pressure, such as during flights.
Diagnosis And Evaluation At Melbourne ENT
At Melbourne ENT, our diagnosis of middle ear infections is thorough and grounded in clinical excellence. We begin with a detailed medical history to understand the nature, frequency, and impact of the symptoms. We ask about recent illnesses, hearing difficulties, speech concerns in children, and any previous treatments or surgeries.
We then conduct a physical examination, including otoscopy – a visual inspection of the ear canal and eardrum using a specialised tool. This allows us to identify signs of infection, such as redness, bulging, or fluid behind the eardrum. We may also use pneumatic otoscopy to assess the eardrum’s mobility, which helps confirm the presence of fluid.
To gain a clearer picture of middle ear function, we often perform tympanometry, which measures the pressure and movement of the eardrum. For children or adults with suspected hearing loss, we conduct audiometry, a painless test to evaluate hearing ability across various frequencies.
In complex or recurrent cases, additional investigations may be required. These include nasal endoscopy to assess the nasopharynx and adenoids, or imaging such as a CT scan if complications are suspected. Our evaluations are always tailored to the patient’s age and specific condition, ensuring accurate diagnosis and a personalised treatment plan.
Treatment Options For Middle Ear Infections
Treatment for AOM is guided by the severity and persistence of symptoms, the patient’s age, and the frequency of infections. In many children, especially those over two years of age with mild symptoms, the infection may resolve without antibiotics. This approach – called watchful waiting – allows the body’s immune system to fight off the infection naturally while managing pain and inflammation with paracetamol or ibuprofen.
When symptoms are severe, persistent beyond 48 to 72 hours, or when the child is very young, we prescribe antibiotics such as amoxicillin. In cases where the patient is allergic to penicillin or has not responded to initial treatment, alternative antibiotics may be used.
For recurrent infections or persistent fluid build-up – known as otitis media with effusion – surgical treatment may be necessary. The most common procedure is myringotomy with grommet insertion. A tiny incision is made in the eardrum to drain the fluid, and a small ventilation tube (grommet) is placed to keep the middle ear aerated and prevent further accumulation.
In some children, particularly those with enlarged adenoids or nasal obstruction, we may recommend adenoidectomy at the same time as grommet insertion. This combined approach improves Eustachian tube function and reduces the recurrence of infections.
When Is Surgery Recommended?
Surgery is recommended when middle ear infections are recurrent or when fluid in the middle ear persists for more than three months and is affecting hearing. Specifically, surgery is considered if a child experiences three or more infections in six months, or four or more in a year. Additionally, if a child has persistent fluid (glue ear) associated with hearing loss, balance issues, or speech delays, grommet insertion is strongly advised.
In adults, surgical treatment is less common but may be necessary when there is a structural issue, such as chronic sinusitis, a retracted eardrum, or a history of trauma. Surgery may also be indicated if repeated antibiotic courses have failed, or if symptoms significantly impair quality of life.
Grommet insertion is a safe and quick procedure, typically performed under general anaesthetic. It offers immediate relief from symptoms and restores normal hearing in most cases. At Melbourne ENT, both Dr Braham and Dr Kleid perform these procedures regularly in well-equipped private hospitals, with meticulous attention to safety, hygiene, and comfort.
Recovery And Prognosis
Recovery following treatment for AOM is usually swift. For children undergoing grommet insertion, most are able to return to normal activities – including daycare and school – within one to two days. The improvement in hearing is often immediate, and many parents notice rapid progress in speech, attention span, and behaviour following the procedure.
Grommets typically remain in place for six to twelve months and fall out naturally as the eardrum heals. During this time, patients may require regular follow-up visits to monitor hearing and assess the position of the tubes. In some cases, particularly when fluid or infections return after the tubes fall out, a second set of grommets may be necessary.
Water precautions may be recommended depending on the type of grommet used and the child’s activity level. While swimming is generally safe, ear plugs or headbands may be advised for prolonged underwater exposure or in chlorinated pools.
For non-surgical cases managed with antibiotics and pain relief, recovery usually occurs within a few days. However, follow-up is still important to ensure that hearing has returned to normal and that there is no lingering fluid or inflammation.
Risks Or Complications If Left Untreated
While many middle ear infections resolve with treatment, delaying care or ignoring symptoms can lead to serious complications. The most common consequence is hearing loss, which – if prolonged – may affect speech and language development in young children. Even temporary hearing deficits can impact learning, social interaction, and confidence.
In cases where pressure builds excessively within the middle ear, the eardrum may rupture. While this sometimes relieves pain by allowing fluid to drain, it can also result in scarring or long-term damage. Persistent fluid build-up can lead to chronic otitis media, where the infection never fully resolves and discharge becomes a constant issue.
Other rare but severe complications include mastoiditis (infection of the bone behind the ear), tympanosclerosis (eardrum scarring), cholesteatoma (abnormal skin growth in the middle ear), and in extreme cases, the spread of infection to the brain or facial nerves.
These risks underscore the importance of early assessment and treatment – particularly for children with developmental vulnerabilities or a history of repeated infections.
Why Choose Your Surgeon
At Melbourne ENT, we believe that the best outcomes are achieved through a combination of expert care, clear communication, and compassionate support. Our surgeons bring decades of experience, advanced training, and a personalised approach to every patient.
Dr Stephen Kleid has been a leader in ENT surgery in Melbourne for over 40 years. As a former Head of ENT at Royal Melbourne Hospital and a senior surgeon at Peter MacCallum Cancer Centre, he is highly skilled in managing complex ear disorders and chronic infections. His academic contributions and involvement in surgical training ensure that his knowledge remains current and his care remains exceptional.
Dr Simon Braham is known for his kind and patient-centred approach, particularly in paediatric ENT care. He consults at several respected hospitals and is widely trusted by GPs, paediatricians, and parents for his expertise in grommet surgery, tonsillectomy, and managing recurrent infections in children. His calm manner and thorough explanations help families feel informed and reassured at every step.
Together, our team at Melbourne ENT is dedicated to improving ear health, preventing complications, and restoring quality of life for our patients.
FAQs About Middle Ear Infection (AOM)
How can I tell the difference between a normal cold and a middle ear infection in my child?
A cold typically causes symptoms like a runny nose, sneezing, and mild fever. When a middle ear infection develops, symptoms often intensify. Your child may suddenly become more irritable, tug at their ears, have difficulty sleeping, and complain of ear pain or show signs of hearing loss. If your child has a fever that persists beyond a few days or seems unusually distressed, it’s best to seek medical advice.
Why does my child keep getting ear infections even after antibiotics seem to work?
While antibiotics can clear up an infection, they don’t address underlying causes like poor Eustachian tube function or enlarged adenoids. If fluid remains trapped in the middle ear, it creates a favourable environment for bacteria to grow again. Some children have anatomy or immune responses that make them prone to recurrence, which is why grommets are sometimes recommended.
Can fluid in the middle ear affect my child’s speech and learning at school?
Yes. Chronic fluid build-up, even without active infection, can cause temporary hearing loss. In young children, this can delay speech development and affect classroom learning, especially in noisy environments. Many children appear inattentive or are misdiagnosed with behavioural issues when hearing problems are the real cause.
Is it normal for my child to still have hearing issues weeks after an ear infection?
It can be. Even after the infection clears, fluid can linger in the middle ear for weeks, affecting hearing. If hearing doesn’t improve after four to six weeks, or if your child has multiple episodes, a hearing test and ENT review are recommended to assess whether intervention is needed.
What should I watch for if my child has had grommets inserted?
After grommet surgery, most children recover quickly with improved hearing and fewer infections. Watch for signs of persistent discharge from the ear, which may indicate an infection around the tube. Also, follow your surgeon’s advice about water precautions and attend regular follow-up appointments to monitor the tubes and hearing.
Are there any activities or environments that might make ear infections more likely to return?
Yes. Frequent exposure to group environments like daycare, especially during cold and flu season, increases the risk. Secondhand smoke, pacifier use beyond infancy, and bottle feeding while lying flat can also contribute. Managing allergies and keeping the nose and sinuses clear can help reduce frequency.
Can adults develop middle ear infections, and are the symptoms different from those in children?
Adults can and do develop middle ear infections, often in conjunction with colds, sinus infections, or barotrauma from flights or diving. The symptoms are generally similar to those in children – ear pain, pressure, reduced hearing, and occasionally fluid discharge – but adults can articulate them more clearly. Persistent or recurrent adult ear infections should always be evaluated, as they may point to underlying structural or sinus issues..
Sources:
- Acute Otitis Media: Practice Essentials, Background, Anatomy – Medscape
https://emedicine.medscape.com/article/859316-overview - Otitis Media: Practice Essentials, Background, Pathophysiology – Medscape
https://emedicine.medscape.com/article/994656-overview - Acute Otitis Media – StatPearls – NCBI Bookshelf
https://www.ncbi.nlm.nih.gov/books/NBK470332/ - Acute Otitis Media Treatment & Management – Medscape
https://emedicine.medscape.com/article/859316-treatment - Acute Otitis Media Guidelines – Medscape
https://emedicine.medscape.com/article/859316-guidelines - Chronic Suppurative Otitis Media – Medscape
https://emedicine.medscape.com/article/859501-overview - Otitis media – Wikipedia (provides comprehensive referenced medical info)
https://en.wikipedia.org/wiki/Otitis_media
Concerned About Middle Ear Infections?
If you or your child is experiencing ear pain, hearing difficulties, or repeated ear infections, it is important not to delay seeking professional help. Early diagnosis and timely treatment by a specialist can prevent long-term complications and significantly improve quality of life. At Melbourne ENT, our expert surgeons provide comprehensive, compassionate care for both adults and children with ear-related concerns. To book a consultation with Dr Stephen Kleid or Dr Simon Braham, please contact the clinic directly or visit the website to learn more.
Further Reading
- Read about Melbourne ENT’s Adenoidectomy
- Read about Melbourne ENT’s Ear Concerns
- Read about Melbourne ENT’s Ear Ache Melbourne
- Read about Melbourne ENT’s Surgery for Ear Tubes in Melbourne
- Read about Melbourne ENT’s Grommets Surgery Melbourne
Why Choose Dr Kleid ?

Dr Stephen Kleid,
Melbourne ENT Surgeon
MED0001052799
Dr Stephen Kleid is an experienced ENT Surgeon (Otolaryngologist) based in Melbourne with a passion for Septo-rhinoplasty, Septoplasty and a strong interest in Rhinoplasty Revision.
Qualifications
- AHPRA (Medical Board)
- MB, BS; FRACS (Fellow of the Royal Australasian College of Surgeons)
- AAFPS – Member of the Australasian Academy of Facial Plastic Surgery
- AAFPRS – (International Member of the American Academy of Facial Plastic and Reconstructive Surgeons)
Dr Kleid’s Procedures
Why Choose Dr Braham ?

Dr Simon Braham,
Melbourne ENT Surgeon
MED0001144757
Dr Simon Braham MBBS (Hons) FRACS is an experienced Ear, Nose and Throat ENT Surgeon (Otolaryngologist) based in Melbourne, performing tonsil, grommet and sinus surgery for children & adults. He helps patients with breathing issues, snoring concerns and sleep disturbances.
Dr Braham’s Procedures
How can we help?
The Melbourne ENT Team takes pleasure in assisting you with any questions when considering a plastic surgery procedure. Please call the St Kilda East clinic in Melbourne between 9am – 5 pm on Weekdays.
What Next?
Want more information about your Procedure?
- Please read our website and blogs to find out more about your procedure and concerns
- For more information about pricing and payment methods, please visit our page on Surgery Payment Options.
- Talk to our Patient Care Team from 9 am to 5 pm Monday to Friday

What to Bring to Your Consultation
- We encourage you to bring a friend or family member to accompany you, as they can provide an extra perspective and support throughout the process.
- It is important to take thorough notes and carefully review all the documents provided to you.

How to Book a Consultation
- A referral from your GP or Specialist is necessary to see a surgeon for a consultation.
- Check the guide to consultation fees and payment for Melbourne ENT plastic surgeons.
- Please contact us to book your consultation.

